Introduction
Diabetes is a group of diseases that affect how your body uses blood sugar or glucose. It was once thought to be just one disease, but now we know that there are different types of diabetes. All types are characterized by having too much sugar in the blood, also known as chronic hyperglycemia. This happens because the body either doesn’t make enough insulin or can’t use insulin properly. Insulin is a hormone that helps the body use glucose for energy. It also controls the metabolism of fats and proteins.
Types of Diabetes
Diabetes Mellitus
1. Type 1 Diabetes (Insulin-Dependent Diabetes Mellitus, IDDM)/ Type 1 DM:
This type is more severe and usually starts in people under 30 years old. It often appears suddenly, and the highest number of cases occur between ages 10 and 14. Type 1 diabetes happens when the body’s immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas (pancreatic beta cells). Without insulin, the body can’t control blood sugar levels. Uncontrolled blood sugar levels can lead to serious health problems if not treated with insulin shots.
2. Type 2 Diabetes (Non-Insulin Dependent Diabetes Mellitus, NIDDM)/ Type 2 DM:
This is the most common form of diabetes. It usually develops gradually in middle-aged or older adults. In Type 2 diabetes, the body still makes insulin but doesn’t use it well. This type is often managed with a healthy diet, exercise, and sometimes medication or insulin.
3. Malnutrition-Related Diabetes Mellitus
This type is less common and is related to poor nutrition, particularly in childhood.
Impaired Glucose Tolerance
This is a condition where blood sugar levels are higher than normal but not high enough to be classified as diabetes. It’s often seen as a “warning sign” that diabetes may develop if lifestyle changes are not made.
Gestational Diabetes Mellitus
This type of diabetes occurs during pregnancy. It usually goes away after the baby is born. But it can increase the risk of developing Type 2 DM later in life.
Understanding Diabetes: A Growing Problem Worldwide
Diabetes is a disease that affects how the body uses sugar, also known as glucose. There are different types of diabetes, but they all lead to high levels of sugar in the blood. High levels of sugar in the blood can cause serious health problems over time. Diabetes is often called an “iceberg” disease because a lot of its effects are hidden beneath the surface. This means that many people may have this condition or be at risk without even knowing it.
Increasing Rates of Diabetes Around the World
The number of people with type 2 DM, which is the most common type, is rising quickly all over the world. This increase is especially noticeable in countries that are growing economically and becoming more industrialized.
According to the 2021 International Diabetes Federation (IDF) Diabetes Atlas, there are 537 million adults between the ages of 20 and 79 worldwide who have diabetes. This means that about 10.5% of adults in this age group have the disease. This number includes people with both type 1 and type 2 DM, whether they’ve been diagnosed or not. The IDF expects that the number of people with diabetes will grow to 643 million by 2030 and to 783 million by 2045. That’s a 46% increase over the next 25 years!
Diabetes in Younger People
In the past, type 2 DM was mostly found in middle-aged and older people. However, now it’s being seen in younger people, including teenagers. “The rate of Type 2 diabetes developing in young people rose from 0.75 per 100,000 patient-years in 2011 to 1.25 per 100,000 in 2019, showing an annual increase of 6.8% (National Library Of Medicine).”
This trend is especially common in groups that are at higher risk due to genetics and lifestyle. In developing countries, many people are getting this disease during the most productive years of their lives. This can create serious challenges for healthcare systems because these people will need medical care for many years to manage the disease and its complications.
Causes of Rising Diabetes Rates
The rise in diabetes, particularly in developing countries, is closely linked to changes in lifestyle and society. Research shows that in Southeast Asia, 20% of the world’s diabetics live in this region. The International Diabetes Federation’s Diabetes Atlas highlights a significant increase in diabetes cases in South-East Asia, projecting a 68% rise by 2045, reaching 152 million people. The report also points out a growing prevalence rate, which is expected to reach 11.3%, alongside challenges like undiagnosed cases and rising healthcare costs related to diabetes.
As countries become more urbanized, people often adopt unhealthy habits like eating processed foods and getting less physical activity. Urban areas also tend to have higher rates of obesity, which is a major risk factor for developing type 2 DM.
Diabetes and Age
The likelihood of developing diabetes increases with age. In South-East Asia, the number of people over 30 years old has been rising, and so has the number of people with this condition. Urban areas have higher diabetes rates than rural areas. Studies show that diabetes is about twice as common in cities as it is in the countryside.
Genetic and Lifestyle Factors
For some people, especially those of Asian descent, genetics can play a big role in developing diabetes. “Asians are more likely than Europeans to develop diabetes at a younger age and much higher rates, even with the same amount of weight gain. Research, including genome-wide association studies (GWAS), has identified over 70 genetic locations linked to Type 2 diabetes, indicating that genetics play a significant role in this increased risk (National Institute of Health)”
When combined with unhealthy lifestyles, like poor diet and lack of exercise, the risk of getting diabetes increases. Recent surveys in countries like Bangladesh, India, and Indonesia have shown that diabetes rates are going up in both cities and rural areas.
Complications
If diabetes is not properly managed, it can lead to many serious health problems. These include heart disease, stroke, kidney disease, nerve damage, and eye problems. These complications can make life very difficult and often lead to early death. It can also cause problems during pregnancy for both the mother and baby.

Lack of Awareness and Challenges in Healthcare
Unfortunately, many people are still not aware of how serious diabetes can be or how to prevent it. There is also a lack of awareness about how to manage diabetes and its complications. In many places, healthcare systems are not equipped to deal with the increasing number of diabetic cases. This can lead to poor diagnosis, inadequate treatment, and insufficient follow-up, causing more severe health issues and early death.
Higher Mortality Rates in Diabetics
People with diabetes have a higher risk of death than those without the disease. This is mostly due to complications like heart disease and kidney problems. In some countries, infections are also a major cause of death among people with diabetes. If the number of people with this condition continues to rise, these health problems could become even more common.
What Causes Diabetes?
Diabetes is a condition that happens when the body can’t properly use sugar, or glucose, which it needs for energy. This issue comes from problems with insulin, a hormone that helps glucose get into our cells. There are two main types of diabetes: Type 1 and Type 2. Understanding what causes these problems and what makes some people more likely to get diabetes can help us learn how to prevent and manage this condition.
Causes of Diabetes (Agent)
The main cause of diabetes is a problem with insulin. In Type 1 DM, the body doesn’t produce insulin i.e. absolute deficiency. On the other hand, in Type 2 DM, the body doesn’t use insulin properly, leading to a “partial deficiency.” Here are some reasons why insulin problems might happen:
Pancreatic Disorders
The pancreas is an organ that plays a crucial role in making insulin. If the pancreas is affected by diseases like inflammation (swelling), tumors, or conditions like cystic fibrosis, it can’t produce enough insulin or make insulin that works properly. This can lead to diabetes.
Defective Insulin Production
In some cases, the body produces insulin, but is abnormal and doesn’t work as it should. This can happen if there’s a problem during the insulin-making process in the body.
Destruction of Beta Cells
Beta cells in the pancreas are responsible for producing insulin. Certain viruses such as mumps and rubella, or chemical agents like arsenic can destroy these cells.
Reduced Insulin Sensitivity
Sometimes, even if the body produces insulin, it doesn’t work effectively because the cells don’t respond to it properly. This is often due to a decrease in the number of insulin receptors on cells, especially in people who are overweight.
Genetic Defects
Some people are born with changes or mutations in their insulin genes that affect how insulin is made or used by the body, making them more likely to develop this condition.
Auto-Immune Problems
In Type 1 DM, the immune system, which usually protects the body from germs, mistakenly attacks and destroys the beta cells in the pancreas. This auto-immune response stops insulin production, leading to high blood sugar levels.
These factors make it harder for the body to use glucose properly, leading to high blood sugar levels, known as hyperglycemia. Over time, high blood sugar can cause serious health problems, like damage to the heart, kidneys, eyes, and nerves.
Who is More Likely to Get Diabetes? (Host Factors)
Several factors can make a person more likely to develop this disease. These are known as “host factors” because they are related to the individual themselves:
Age
Although diabetes can happen at any age, it’s more common as people get older. For example, Type 2 DM usually starts in middle age or later.
However, malnutrition-related diabetes, which is linked to poor nutrition, often affects younger people. In early childhood, not getting enough protein can cause the beta cells, which help control blood sugar, to stop working properly. If a child continues to have low protein intake, this can lead to diabetes at a young age. Unfortunately, once this damage happens, it might not be reversible.
The older someone gets, the higher the risk of developing diabetes because the body’s ability to use insulin can decrease over time.
Gender
In some countries, diabetes rates are about the same for men and women. However, in parts of South-East Asia, more men are reported to have diabetes. This might be due to differences in lifestyle, diet, or genetic factors.
Genetics
Diabetes can run in families, meaning it can be passed down from parents to children. For example, if one identical twin has Type 2 DM, there’s about a 90% chance the other twin will get it too. For Type 1 DM, this chance is around 50%. This shows that genetics play a strong role in developing this disease.
Genetic Markers
Some people have specific genetic markers (HLA-B8, HLA-B15, HLA-DR3, and HLA-DR4) that make them more likely to develop Type 1 DM. These markers are found in genes related to the immune system. People with certain combinations of these markers are at a higher risk. On the other hand, Type 2 DM is not associated with HLA.
Immune System Issues
Some people have immune systems (cell-mediated and humoral immunity) that mistakenly attack their insulin-producing cells, especially if triggered by environmental factors like viruses or certain chemicals. This is more common in Type 1 DM.
Obesity
Being overweight and obese, especially carrying extra weight around the belly, is a big risk factor for Type 2 DM. This is because excess fat, particularly in the abdominal area, can make the body less sensitive to insulin. This is known as insulin resistance, meaning the body’s cells don’t respond well to insulin. Studies have shown that as body mass index (BMI), waist circumference, and waist-to-hip ratio increase, so does the risk of developing Type 2 diabetes. Losing weight through diet and exercise can improve insulin sensitivity and lower the risk of diabetes.
Maternal Diabetes
Children born to mothers with diabetes, including gestational diabetes, are at higher risk of developing this condition themselves, especially if they are born large or gain weight quickly as they grow. If a mother develops diabetes before giving birth, her child is three times more likely to develop the disease compared to a child born before she developed the condition. If a baby is born underweight due to the mother’s diabetes, and then gains weight rapidly after birth, this can also increase the risk of developing the disease later in life.
Environmental Factors That Increase the Risk of Diabetes
Certain lifestyle and environmental factors can increase the risk of developing diabetes, especially for those who already have a genetic predisposition:
Sedentary Lifestyle
Not getting enough physical activity can increase the risk of Type 2 DM. Physical activity helps the body use insulin more effectively, so a lack of exercise can lead to insulin resistance. Studies have shown that people who lead a sedentary lifestyle are more likely to develop diabetes than those who are active.
Diet
Eating a diet high in saturated fats (like those found in fast food, red meat, and butter) and low in fiber can increase the risk of diabetes. Diets high in saturated fats can lead to higher fasting glucose and insulin levels. Higher insulin levels are markers of insulin resistance and diabetes. On the other hand, eating healthy fats from vegetables and fish and high-fiber foods like whole grains, fruits, and vegetables can help lower this risk. These foods help improve insulin sensitivity and control blood sugar levels.
Dietary Fiber
Fiber is an important part of a healthy diet. Eating a diet high in dietary fiber reduces blood glucose and insulin levels in people with Type 2 DM and those with impaired glucose tolerance (a condition that often leads to this condition). Experts recommend a diet rich in whole grains, vegetables, and fruits to help prevent diabetes.
Malnutrition
Poor nutrition during childhood, known as malnutrition, can affect how the body manages glucose and insulin, increasing the risk of diabetes later in life. Malnutrition can cause the beta cells in the pancreas, which produce insulin, to not function properly.
Alcohol
Drinking too much alcohol can damage the pancreas and contribute to obesity, both of which increase diabetes risk. Excessive alcohol consumption is a known risk factor for Type 2 DM.
Viral Infections
Certain viruses like rubella, mumps, and coxsackie virus B4 have been linked to the development of diabetes in genetically susceptible people. These viruses can trigger an immune response that mistakenly attacks the insulin-producing cells in the pancreas.
Chemical Agents
Some chemicals can be toxic to the insulin-producing cells in the pancreas, increasing the risk of diabetes. For example, chemicals found in certain foods, like cassava and some beans, can produce substances that are harmful to the pancreas.
Stress
High stress from situations like surgery, trauma, or emotional stress can sometimes trigger diabetes in people who are at risk. Stress can affect how the body uses insulin and can lead to higher blood sugar levels.
Other Social Factors
Social factors such as occupation, education, economic status, and lifestyle changes can also influence the development of this condition. In many places, diabetes is now more common in lower-income groups, which wasn’t the case 50 years ago. This shift may be due to rapid lifestyle changes, like eating more processed foods and getting less physical activity. Lower-income groups may also have less access to healthy foods and healthcare, increasing the risk of this disease.
Understanding these causes and risk factors can help us take steps to prevent this disease and manage it effectively if it occurs. By maintaining a healthy lifestyle, staying informed, and making regular visits to the doctor, we can reduce the chances of developing this condition and improve overall health.
Signs and Symptoms of Diabetes: What to Watch For
Diabetes can come with a variety of signs and symptoms, and it’s important to recognize them early. Common warning signs include frequent urination, excessive thirst, and unexplained weight loss. You might also notice increased hunger, blurry vision, and extreme fatigue.
Other symptoms can include slow-healing wounds, frequent infections, and tingling or numbness in the hands and feet. If you experience these symptoms, it’s a good idea to see a healthcare provider for a check-up and blood sugar test to rule out diabetes. Early detection is key to managing the condition effectively.
Screening For Diabetes
Screening for diabetes involves checking people who don’t show any symptoms to see if they have high blood sugar levels. In the past, one of the most common methods for screening diabetes started with a simple test to check for glucose (a type of sugar) in a urine sample. If glucose was found, the person would then take an oral glucose tolerance test to confirm. The goal was to find diabetes early and manage it before any symptoms appeared, helping to reduce the risk of complications.
Urine Examination
One method used in medical practice to detect diabetes is testing urine for glucose about 2 hours after a meal. If glucose is found in the urine, it suggests that the person might have diabetes, and further testing, like a standard oral glucose tolerance test, is needed to confirm it.
However, urine tests have some limitations. Studies have shown that while urine tests can detect glucose in more severe cases of diabetes, they often miss milder cases where glucose isn’t present in the urine. This means the test lacks “sensitivity.” Sensitivity refers to how well a test can correctly identify those who actually have the disease. For urine glucose tests, sensitivity can be quite low, ranging from 10% to 50%. This means that many people with this disease might not be detected if only a urine test is used, leading to a high number of “false negatives.”
Blood Sugar Testing
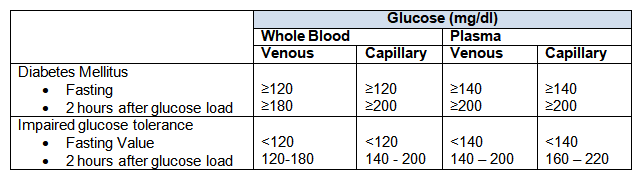
Because urine tests have their limitations, the “standard oral glucose tolerance test” has become the main method for diagnosing diabetes. In large screening programs, blood glucose levels can be measured in different ways: fasting (when the person hasn’t eaten for several hours), after a meal (post-prandial), or using a random blood sample taken at any time.
However, measuring glucose from random blood samples isn’t very reliable for large population studies.
Testing blood glucose levels after fasting can also be tricky because ensuring that everyone truly fasts (doesn’t eat or drink anything other than water) before the test can be hard. This can sometimes lead to incorrect diagnoses of this condition.
To get more accurate results, especially in studies that examine the health of entire populations, researchers usually measure blood glucose levels two hours after a person drinks a solution containing 75 grams of glucose. They can use this method, known as the oral glucose tolerance test, alone or combine it with fasting glucose measurements for better accuracy.
With the help of automated biochemistry, it’s now possible to screen thousands of blood samples for glucose quickly and efficiently. The World Health Organization (WHO) has established specific guidelines for diagnosing diabetes based on these glucose measurements, making it easier for healthcare providers to identify and manage the condition.
Target Population for Screening
Screening the entire population for diabetes is generally not considered effective or practical. Instead, it’s more beneficial to focus on screening “high-risk” groups who are more likely to develop the disease. These high-risk groups include:
- People aged 40 and older.
- Individuals with a family history of diabetes.
- Those who are obese.
- Women who have given birth to a baby weighing more than 4.5 kg (or 3.5 kg in populations where people are generally smaller).
- Women who gain excess weight during pregnancy.
- Patients who have early signs of atherosclerosis (hardening of the arteries).
By focusing on these high-risk groups, healthcare providers can better identify individuals who may benefit from early intervention and management of diabetes.
Prevention and Care
Primary Prevention
Preventing diabetes, especially Type 2 DM, is possible through a couple of key strategies: (a) a population-wide approach and (b) a high-risk approach.
1. Population Strategy
For Type 1 DM, there are still limited options for prevention because we don’t yet have enough knowledge about how to prevent it. However, when it comes to Type 2 DM, there are clear steps we can take to reduce the risk, especially by focusing on environmental factors.
In countries where these risk factors haven’t become common yet, there’s a strong need for what’s called “primordial prevention.” This means stopping these risk factors, like poor diet and lack of exercise, from developing in the first place.
To prevent Type 2 DM on a larger scale, it’s important to encourage people to maintain a healthy body weight through good nutrition and regular exercise. This involves eating a balanced diet that includes enough protein, plenty of fiber-rich foods like fruits, vegetables, and whole grains, and avoiding too many sugary foods. In some areas, it might also be necessary to address specific issues like protein deficiency and exposure to food toxins. These preventive measures should be part of larger community programs that also aim to prevent other non-communicable diseases, like heart disease.
2. High-Risk Strategy
Currently, there isn’t a specific high-risk prevention plan for Type 1 DM. Genetic counseling, which involves advising people about their risk based on their family history, isn’t considered practical for preventing Type 1 DM at this time.
For Type 2 DM, the high-risk strategy focuses on individuals who are more likely to develop the disease due to factors like a sedentary lifestyle, overeating, and obesity. To reduce their risk, people in these groups should try to stay active, eat a healthy diet, and avoid gaining excess weight. It’s also recommended to avoid alcohol, as it can indirectly increase the risk of diabetes. People at risk should also avoid medications that can raise blood sugar levels, like certain oral contraceptives.
Additionally, it’s important to reduce factors that can lead to atherosclerosis or the hardening of the arteries. This includes avoiding smoking, controlling high blood pressure, lowering high cholesterol, and managing high triglyceride levels. By focusing on these high-risk groups, we can more effectively prevent the onset of Type 2 DM and reduce its complications.
Secondary Prevention
Once the disease is diagnosed, it’s important to manage it effectively to prevent complications. The main goals of diabetes treatment are to (a) keep blood glucose levels as close to normal as possible, and (b) maintain a healthy body weight.
Treatment options vary based on individual needs and can include:
- Diet Alone: Eating small, balanced meals more frequently throughout the day to manage blood sugar.
- Oral Antidiabetic Drugs and Diet: Using medications alongside a healthy diet to help control blood sugar levels.
- Diet and Insulin: Combining insulin injections with proper dietary management.
Proper control of blood sugar is essential to avoid complications. Regular monitoring of various health indicators is key to managing this disease effectively.
Monitoring and Management
Managing diabetes well means keeping a close eye on several health factors:
- Blood Sugar Levels: Regular checks are necessary to make sure blood glucose levels stay within the target range.
- Urine for Proteins and Ketones: Testing for these substances can help detect early signs of kidney problems or high blood sugar.
- Blood Pressure: Keeping blood pressure under control is crucial to prevent complications like heart disease.
- Visual Acuity: Regular eye exams are important because diabetes can lead to vision problems over time.
- Weight: Maintaining a healthy weight can improve blood sugar control and overall well-being.
- Foot Health: Regularly checking for good blood circulation, loss of sensation, and skin health is important to prevent foot problems, which are common in people with diabetes. Tools like Doppler ultrasound probes can help assess blood flow in the feet.
Primary healthcare plays a vital role in managing diabetes because most patients receive their care at this level.
Glycosylated Hemoglobin (HbA1c)
People with this condition should get their glycosylated hemoglobin (HbA1c) levels checked every six months. The HbA1c test gives a long-term picture of blood glucose control by measuring the amount of glucose attached to hemoglobin in red blood cells. Since red blood cells live for about 2-3 months, the HbA1c level shows average blood glucose levels over that period.
Self-Care
Self-care is a crucial part of managing this condition. People with diabetes should take responsibility for their care with guidance from healthcare professionals. Key aspects of self-care include:
- Following Diet and Medication Plans: Sticking to the recommended diet and taking prescribed medications as directed.
- Monitoring Urine and Blood Glucose: Regularly check urine for glucose and, if possible, use a home blood glucose monitor to track blood sugar levels.
- Insulin Administration: For those who need it, learning how to administer insulin correctly is important.
- Avoiding Alcohol: Staying away from alcohol, which can affect blood sugar levels.
- Maintaining a Healthy Weight: Working towards and keeping an optimal weight.
- Regular Check-Ups: Going to scheduled medical appointments for regular health checks.
- Recognizing Symptoms: Knowing the signs of high blood sugar (glycosuria) and low blood sugar (hypoglycemia) and understanding how to respond.
Home Blood Glucose Monitoring
Thanks to recent advancements, it’s easier than ever for people with this condition to monitor their blood sugar levels at home. Devices like glucose meters and test strips allow for quick and reasonably accurate blood glucose measurements from a drop of blood, helping people manage their condition more effectively.
Patient Education
People with diabetes need to understand their condition and how to manage it effectively. Diabetic patients should carry an identification card with their details and information about their treatment. Education is key, not just for patients but also for their families, to make the most of primary healthcare services and ensure good diabetes management.
Tertiary Prevention
This disease can lead to serious complications that cause disability, such as blindness, kidney failure, heart attacks, and gangrene in the lower limbs. The main goal of tertiary prevention is to manage these complications and prevent them from getting worse. This involves setting up specialized clinics, known as diabetic clinics, that have the expertise to provide advanced diagnostic and treatment services.
There is a significant need for these specialized clinics in large towns and cities to ensure that people with diabetes can access the care they need. These clinics are also important for conducting basic, clinical, and epidemiological research to better understand this disease and its complications.
Additionally, it is recommended that local and national registries for people with this disease be established. These registries can help keep track of patients, improve the quality of care, and support research efforts to develop better treatment strategies.
Conclusion
Managing this condition effectively requires understanding its causes, risk factors, and various preventive strategies. Early detection through proper screening methods is essential to prevent complications and maintain quality of life. With the right lifestyle choices, such as a balanced diet, regular exercise, and routine health check-ups, many individuals can significantly reduce their risk of developing high blood sugar levels and related health issues. It’s also important to recognize the value of both self-care and professional medical guidance in managing symptoms and maintaining overall health. By staying informed and proactive, people can lead healthier lives and minimize the impact of this chronic illness.
